The lives of Rachel and Andreas Simon
Sunday, September 26, 2010
Peri schmeri, who needs em?!
My Friday appointment with the peri was ridiculous. I feel like every time I get information from one OB, it's completely contradicted by another. It leads me to believe that, instead of being lead by fact, they are simply being lead by opinion. Some OBs are just stuck in their ways, won't venture outside the box, or are too lazy to keep up with current research. Blah. I've had it.
Nevertheless, I feel compelled to share a little about some of the things my peri was saying while at the appointment. And for the record, I will also say that I came into the appointment under the pretense of decreased fetal movement due to cord entanglement (which I said for billing purposes only, although she is entangled in her cord).... well, they kept me waiting in the lobby for over an hour. Now what does that tell you? At any rate, doc wasn't surprised to see me. I think I give him so much grief at every appointment, that he just expects my visits once a week. One of the reasons I am able to give him so much grief is because I'm not one of those acquiescent, naive moms who takes everything he says as kosher. I'm a PhD student in Biology, so I know what research is and how it's conducted. He can't be blowing smoke up my maternity shorts.
The appointment started off as it typically does- I relayed my worry about the cord being wrapped around the baby, said she's having decreased movements, he starts the ultrasound, confirms where the cord is (same place as Dr Collins found it), and then launches into his well rehearsed speech about how everything I'm seeing and feeling (regarding cord stuff) is normal. "The cord can't be floating in front of the baby the entire pregnancy", "The cord placement is totally normal- we see it draped over the baby's neck and between the baby's legs all the time", "The so called cord compressions you speak of are normal in every pregnancy- they aren't cord compressions, rather the reaction of the sympathetic and parasympathetic nervous system to a halt in movement".... I had made the mistake of telling him that I flew to Louisiana to meet with Dr Collins, who has been studying cord accidents for over 20 years, in order to start the home monitoring. He called Dr Collins a "quack", "not a real OB", the list goes on. I couldn't believe the statements that were coming out of his mouth. I even photocopied all of the paperwork Dr Collins gave me regarding cord pathology, but the peri refused to take it from me. I went into his office and left it on his desk, telling him that he needed to look Dr Collins's Pregnancy Institute website up and read all of his peer-reviewed studies. He ended the conversation by saying, "any quack can have a website".
That was enough for one day. I felt like I was leaving the circus. I did march on up to reception though and make weekly appointments for non-stress tests and 2D ultrasounds for the next 5 weeks. I will also be getting my steroid shots and an amnio before 36 weeks. I will have this live, healthy baby in my arms, even if I have to personally mow down the entire OB community to get my way. Ain't nobody gonna hold me down.
Labels:
Baby,
Doctors,
Dr Collins,
Home monitoring
Wednesday, September 22, 2010
If he says no, just come to me.
I had a great appointment with my OB this morning. Essentially, she said that if my perinatologist won't do something I think I need to have (for example, a non-stress test before 32 weeks), we will go around him. "If he says no, just come to me"--sweetest sound to my ears. She's willing to do it all- NSTs whenever I want, checking me into the hospital for as long as I want, giving me steroids to help mature the baby's lungs, giving me an amnio at 32 weeks to check lung maturity, helping me go into labor... she's so freaking awesome. I also got my husband to call that administrator and get the DL on my account info and *exactly* how to use the home monitor.
Ah. I've momentarily been put as ease. I can breathe. Thank goodness. I was ready to check myself into the loony bin.
Ah. I've momentarily been put as ease. I can breathe. Thank goodness. I was ready to check myself into the loony bin.
Labels:
Baby,
Doctors,
Home monitoring
Tuesday, September 21, 2010
Quick update
I've been battling with this home monitor since Sunday afternoon. Dr Collins said it would take a week or so to get it 'working smoothly', and I had no idea what he meant (how hard could it be?!) until I actually tried to transmit a file. Problems I've encountered thus far: not having a landline to hook the modem up to (who runs things through landlines nowadays?), keeping a consistent heart rate with that huge probe doppler thing (it's pretty clumsy for a hospital grade piece of medical equipment), not being able to track down the administrator that sets up my account (he's so damn elusive!), not being able to transmit the files properly (why is the machine shutting off and turning back on by itself?), not being able to login to my account (is it even set up yet?)... blah, blah, blah.
Nonetheless, there are two pieces of good/decent news: 1) I must have done something right with the transmission (after having multiple tantrums and frustration cries) because Dr Collins was able to successfully view my first strip (although he didn't get the text message alert notifying him that I have uploaded a strip- administrator, where are you?) and, 2) the baby's heart rate sounded good. She continues to have some cord compression (so it's somewhere on her body), but Dr Collins does not consider them 'decelerations' per say. I guess I have to relish the good news, even if they are just minor things. Man, I think I need a glass of wine....
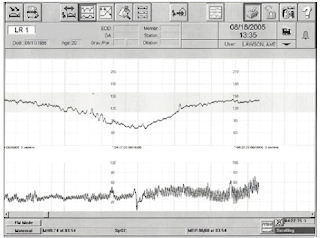
N.B. This is not my strip (cos I can't access mine right now!). This strip shows a major deceleration and would require delivery.
N.B. This is not my strip (cos I can't access mine right now!). This strip shows a major deceleration and would require delivery.
Labels:
Baby,
Doctors,
Dr Collins,
Home monitoring
Sunday, September 19, 2010
It's official. Thank G-d for Dr Collins.
Well, it's official. Officially sad and tragic actually. Cord issues DO recur in subsequent pregnancies. I'm living proof (amongst the other 1200 women who've been studied!). For those of you who aren't aware, my beautiful and flawless daughter, Shiloh, was born sleeping at 39 weeks, 5 days gestation due to an umbilical cord accident in Oct 2008. The cord was wrapped so tightly once around her neck (nuchal cord) and once around her body (body loop) that my OB couldn't even slide her fingers underneath it to free Shiloh after she was born. Her arms and neck were indented from the pressure of the very organ that was meant to sustain her life in utero. How ironic. *As I write this, tears are streaming down my face. Did this really happen to my daughter?* I miss her terribly.
Now, I'm pregnant with number 2. A little sister for Shiloh. I only wish she were here to experience it. I've been conflicted the entire 28 weeks. I'm scared out of my mind (which I previously thought was unsubstantiated, but due to prior experience). I wake up 5 times a night to make sure she hasn't passed away during my sleep. I freak out and think the worst if she is moving too much or too 'hard'. I contemplate running to the hospital every time she has the hiccups (yes- hiccups are ONLY related to cord compression. If your baby has hiccups, the cord IS being compressed one way or another, at least at certain times). Sometimes, when I'm really deluded, I even think this baby is Shiloh, that I've been given another chance with her (I haven't told ANYONE this before, and I feel awful just saying it). Yes. I'm a full-blown nut job and it's starting to wear thin on my being.
But the point of this post is actually to write about my appointment with Dr Collins. I just returned from my trip to Louisiana (a few hours ago!) to meet with Dr Collins regarding the home monitoring for this baby. He is such a passionate, caring man and one that truly wants to rid the world of unnecessary infant death. So, he gave me an ultrasound and hooked me up to the monitor for 30 minutes to check the baby's heart rate and to see if I am having contractions. I'll just get to the point- he confirmed my worst fears. There is cord compression (the baby has been having hiccups 2-3 times per day for 5-10 minutes each for the last 2 weeks) and she’s even having minor decelerations. The cord is possibly being compressed in one or all of three different places. Right now, it is between her legs, around her back and draped over her neck. It's not 360 degrees around any body part, but it's enough to cause her to lay on it or squeeze it at certain times. Now, the decelerations are only 10-30% and she only had 10 in 30 minutes, so he says the baby is ok for the moment, but if it gets worse- 50% and 30 in 30 minutes- I need to deliver. He wants me to get weekly, high-resolution ultrasounds to see what the cord is doing. So my fears are substantiated and now I'm beyond terrified. I want to get this baby out now. A.L.I.V.E.
My OB is totally on board with whatever I want to do, but my perinatologist (who has the high resolution U/S) is not. I had to jump through hoops at 25 weeks to get him to do another U/S to check where the cord was. I begged him to start the non-stress testing at 32 weeks, instead of 34 (which was a compromise- I wanted to start at 30). He believes that the published work on stillbirth is not peer reviewed and has a biased population. He doesn't believe that cord accidents recur and doesn't make an effort to read the available literature (of which there is plenty, which has been peer reviewed by over 30 medical academics, thank you Dr Collins). I'm über-worried because I know he's going to resist when I tell him I need weekly ultrasounds. I feel a tiny bit confident that I will have the home monitor to fall back on for more accurate self-interpretation, but I'm still scared out of my mind. I need the support of these OBs and the hospital, not for them to put up a force field, and I hate that I have to singularly be so damn proactive. Doesn’t everyone want a baby to be born alive if its demise can easily be prevented? I’ll never understand how ignorance can be blissful for the medical community.
To be continued….
Labels:
Baby,
Doctors,
Dr Collins,
Home monitoring
Sunday, September 5, 2010
LoveLE Maternity Photos
My 'LoveLE' friend, Autumn, an aspiring maternity photographer, took some maternity photos of me last week (25 weeks). Here are a few for your viewing pleasure.
Subscribe to:
Posts (Atom)
Blog Design by Gisele Jaquenod